Diagnosing Trich in Children: It Takes A Specialist

Online test
Find out the severity of your symptoms with this free online test
While not at all uncommon, a child losing their hair can be concerning for parents. When it happens, the first stop is usually their pediatrician or dermatologist. But what happens when you have a skin condition that is related to a mental health disorder? Can they still help?
Unlike dermatological conditions that cause hair loss, trichotillomania (TTM) is a body focused repetitive behavior (BFRB) characterized by repetitive hair pulling that results in hair loss, emotional distress, and impaired functioning. TTM is a psychiatric disorder related to obsessive compulsive disorders. It is not a dermatological disorder but does have dermatological implications.
So just how do clinicians determine why someone is pulling their hair and how to treat it? They need a set of tools and skills that can look beyond the hair loss and consider the underlying dynamics. A new study takes a closer look at this intersection of medical and psychiatric care and tools that can be helpful for diagnosing TTM.
Diagnosing Trichotillomania
As with many conditions, there is no single “test” or “sign” that clearly indicates a diagnosis of TTM. Rather, clinicians rely on a number of clinical indicators that, when present together, are indicative of hair pulling. Some of the many tools they may use include:
Clinical presentation – Clinical presentation is essentially how the person presents to their provider (e.g., hair loss, skin lesions) and how they the problem they’re seeking help for. Sometimes, hair loss might be visibly present but not the patient’s complaint. For example, with younger patients, there may be GI issues (possibly indicative of a trichobezoar) or school refusal. The clinical presentation can tell the provider a lot about what’s happening and guide the provider’s diagnosis and choices for treatment. It’s a part of diagnosis that almost every clinician in every discipline relies on.
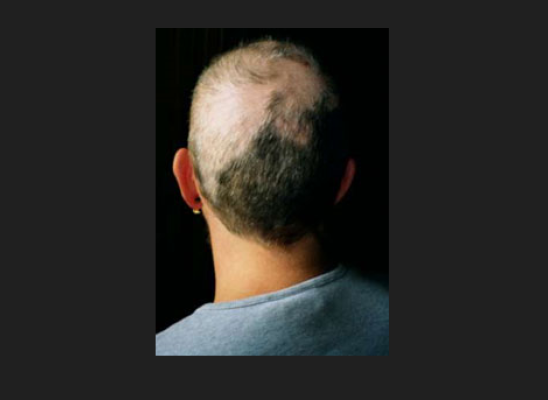
Patterns of hair loss – Hair loss often occurs in distinct patterns, depending on the reason for the loss. TTM typically presents with patches of hair loss on the scalp, eyelashes, eyebrows or beard, and sometimes even the pubic area. The scalp is the most common site for pulling and may leave bald patches on top. Hair on the back of the head is harder to reach and may remain intact. Hair density will be normal.
A detailed history – Taking a detailed medical and psychosocial history can help to identify the onset and progression of the hair pulling. Often thought of as a teen or young adult issue, onset for TTM is bimodal with onset at about 7-8 years old and a second onset at puberty. A complete history can also help identify the situations, triggers, co-occurring conditions, pulling behaviors and rituals, and their consequences that may contribute to the hair pulling.
When seeking to hair pulling in children, it’s important to consider their early experiences. Hair pulling can emerge at different times during the developmental continuum and present in different ways. There is also substantial evidence to suggest that Adverse Childhood Experiences (ACEs) may be related to the emergence of mental health issues including hair pulling. Findings suggest that there may be sensitive “windows” when the experience of trauma or other adverse events can be particularly damaging.
Assessments and scales – There are a number of scales, questionnaires and assessments that can help assess TTM. Some of these may be completed by the patient or in the case of a young child, their parent. Examples include:
- TTM scale for children (a self-report questionnaire)
- National Institute of Mental Health (NIMH) TTM Questionnaire (clinician rated scale)
- Milwaukee Inventory of Subtypes of TTM (MIST) (identifies the type of pulling style)
- Massachusetts General Hospital Hairpulling Symptom Severity Scale (self-report)
Testing – Repeated hair pulling leaves clues.
Visual exam - There may be sites of old growth, missing hair, and new growth. The hairs tend to be broken or distorted, and there may be tiny bleeding points or lesions where hairs have been plucked.
Pull Test – This test involves a gentle pull of the hair. A pull that yields more than 10% of the sample suggests something other than TTM.
Dermoscopy/Trichoscopy – This exam provides an up-close look at the scalp and can identify some of the “tell-tale” signs of TTM such as the presence of “flame hairs” (hair residue that remains after pulling), the “V-sign” (two hairs broken in the same spot and rising from the same follicle), and “tulip hairs” (tiny hairs with dark, tulip-shaped ends).
Assessing for Co-occurring Conditions
TTM often occurs along with other mental health disorders including depression, anxiety, and other body-focused repetitive behaviors (BFRBs) such as skin picking. Having TTM along with a comorbid mental health disorder can result in more severe symptoms of TTM including more severe hair pulling, poor control, greater impairment in functioning, and reduced quality of life.
Treating Hair Pulling
TTM is generally considered to be a chronic condition that can be managed. To date, the gold standard for treating TTM is Habit Reversal Training (HRT). Because BFRBs like hair pulling also have both behavioral and cognitive components, there are emerging approaches that combine HRT with elements of other more cognitively-based treatments such as Acceptance and Commitment Therapy (ACT). Combining these evidence-based approaches may increase the effectiveness of these treatments. More effective treatments mean more positive outcomes and improved quality of life for people living with BFRBs.
A substantial number of people with TTM also have comorbid mental health disorders that may require treatment as well. Treating comorbid disorders may also help to alleviate some of the severity of the hair pulling too.
The Rise of Psychodermatology
In response to the growing recognition that diagnosing psychodermatological disorders requires specific tools and skills, the medical community has responded. Psychodermatology is an emerging field that brings together both the medical and psychiatric expertise needed to treat disorders like hair pulling.
Psychodermatology is redefining dermatological treatment for TTM. It is creating an approach to care that is holistic and cognizant of the connection between the mind and the skin. It is allowing dermatologists to better understand, assess and treat even their littlest patients with confidence and support from behavioral health.
The Takeaway
Of course, every case is different in its presentation and in the tools a clinician might need to use. Depending on a patient’s diagnosis and needs, clinicians may also coordinate with other providers such as psychotherapists or psychiatrists to ensure a complete treatment approach that addresses both medical and psychiatric needs.
There are clinicians who are skilled in caring for people living with disorders like hair pulling. There are treatments that can offer relief. Research continues to search for innovative and effective treatments with the goal of a cure. Hope remains and there is help and support available.
References
1. Thakkar, S., & Desai, N. (2023). Trichotillomania in children − how can a dermatologist deal with it? Indian Journal of Paediatric Dermatology, 24(2), 109-115. https://journals.lww.com/ijpd/Fulltext/2023/24020/Trichotillomania_in_Children___How_can_a.1.aspx?context=LatestArticles
2. Santhanam, R., Fairley, M., & Rogers, M. (2008). Is it trichotillomania? Hair pulling in childhood: A developmental perspective. Clinical Child Psychology and Psychiatry, 13(3), 409-418. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1013.6972&rep=rep1&type=pdf
3. Yasir, W., Sherin, M., & Kazmi, S. F. (2021). The Role of Childhood Trauma in Developing Nail Biting and Trichotillomania Among Adolescents. International Journal of Innovation, Creativity and Change, 15(2), 1314-1332. https://www.ijicc.net/images/Vol_15/Iss_2/17132_Kazmi_2021_E1_R1.pdf
4. Rakowska, A., Slowinska, M., Olszewska, M., & Rudnicka, L. (2014). New Trichoscopy findings in trichotillomania: Flame hairs, V-sign, hook hairs, hair powder, tulip hairs. Acta Dermato Venereologica, 94(3), 303-306. https://medicaljournalssweden.se/actadv/article/view/6339
5. Houghton, D. C., Maas, J., Twohig, M. P., Saunders, S. M., Compton, S. N., Neal-Barnett, A. M., … Woods, D. W. (2016). Comorbidity and quality of life in adults with hair pulling disorder. Psychiatry Research, 239, 12-19. https://www.sciencedirect.com/science/article/abs/pii/S0165178116303614?via%3Dihub
6. Capriotti, M. R., Ely, L. J., Snorrason, I., & Woods, D. W. (2015). Acceptance-enhanced behavior therapy for excoriation (skin-picking) disorder in adults: A clinical case series. Cognitive and Behavioral Practice, 22(2), 230-239. https://www.academia.edu/29681898/Case_Study_about_Excoriation_Skin_Picking_Disorder_
Online test
Find out the severity of your symptoms with this free online test
Start your journey with TrichStop
Take control of your life and find freedom from hair pulling through professional therapy and evidence-based behavioral techniques.
Start Now